Learning to Live With Low Vision:
One Man’s Journey Through Rehabilitation
Transcript
(Free distribution allowed with proper credit given)
This is a dramatization of the experiences of Jim, a fictional participant in a low vision rehabilitation program. The intent is to introduce the reader to as many of the varied types of tests and interventions as possible. For simplicity, a single character has been used to show many possible approaches. It does not, therefore, necessarily represent a typical case.
Since individual programs will be geared to each person’s unique capabilities and goals, evaluation and training may be expected to include some, but not all of the options presented here.
Jim’s Story
I thought maybe there was a smear on my glasses, so I took them off. But that smudge was still there, right in the middle of my left eye. And when I looked at the frame around the board, it was all out of shape…distorted. I don’t know why I hadn’t noticed it before. I couldn’t blink that spot away, or rub it away, or anything. It was just there, and I didn’t know what was going on.
I was supposed to attend a staff meeting that afternoon, but I didn’t. I just left. I had to find out what was going on, so I went straight home and called my optometrist. He made time for me that afternoon. To make a long story short, I knew in a few hours that I had an eye disease I never heard of and couldn’t even pronounce. I had become one of the vision-impaired, and I was off on a trip I had never in my life expected to take.
This essay will take you with me as I retrace that journey. It will show you how a program of low vision rehabilitation training can help you to live successfully with sight loss. My hope is that, by having this information early on, you will not have to experience the emotional distress and sense of helplessness that I did when I first faced a future with vision impairment.
What Is Vision Impairment?
An estimated fourteen million Americans are vision-impaired, but only about 120,000 are classified as “totally blind.” This means that a very large percentage of those millions can benefit from low vision rehabilitation.
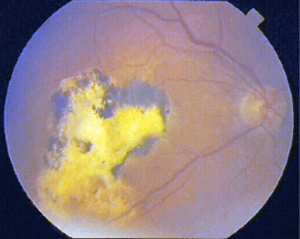
With the population growing older and living longer, the total number of vision-impaired people is dramatically increasing. Some 2.5 million patients, for example, are newly-diagnosed each year with macular degeneration, a yet incurable disease of the retina that is the leading cause of vision loss in senior citizens. This is serious, not only on a personal level, but for society as a whole. Each year, the vision-impaired community costs the United States more than 22 billion dollars in education expenses, income loss, services, and government disability programs.
An obvious solution to the problem would be a cure for retinal disease coupled with ways to restore lost sight. These developments will be a reality in the future, but until then, the most effective approach has proven to be education and training for the vision-impaired through good rehabilitation programs.
Vision impairment is generally any interference with sight that hinders the performance of daily activities. More specifically, vision impairment is a term which describes varying degrees of vision loss caused by disease, trauma, or a congenital disorder.
Vision impairment may appear as one or more of six general conditions:
Blurriness, where visual acuity with best spectacle correction is still reduced or blurred;
A person who meets one of these criteria might still have usable vision, but he would not be able to read without training on an assistive device. Also, he would not be able to meet the requirements for obtaining a driver’s license. This person would be described as vision-impaired, but another person who is vision-impaired may not necessarily be legally blind.
Strategies for individuals with total blindness must be non-visual. Many times, vision-impaired individuals will also benefit from non-visual solutions for improved accuracy and efficiency with a variety of tasks. The worse the vision, the greater will be the reliance on non-visual techniques and devices.
With diseases that affect the peripheral, or side field, mobility is more seriously affected. Glaucoma, retinitis pigmentosa, and stroke, for example can constrict the visual field to as little as 10 to 15 degrees. Even with this severe limitation, however, rehabilitation can successfully reinforce the individual with training in the use of low vision devices.
What Is Low Vision Rehabilitation?
Low vision rehabilitation is like physical therapy for someone who has lost a limb. Its purpose is to develop strategies to maximize or substitute for diminished sight in order to maintain independence and a sense of self-worth. This rebuilding and reinforcement of the visual foundation is accomplished through identification of goals, introduction to assistive devices, and training.
Rehabilitation is not just an introduction to low vision devices. Actually, that may not occur until some time into the program, after the patient has gone through evaluation and training. Only then can appropriate recommendations for low vision devices be made.
Depending upon the patient’s needs, a good program might also provide education, support groups, and individual counseling. It would help the patient to realize that using such devices and techniques is a sign of tenacity and courage, not weakness or defeat.
People with a constricted visual field might expect to be introduced to scanning therapy and devices such as visual field awareness prisms and reverse telescopes. People with severe vision loss should expect to receive orientation and mobility training, occupational therapy, and information about animal guides and occupational therapy.
In addition to these skills, vision rehabilitation specialists teach how to manage daily activities such as:
- adapting the home for safety and navigation;
- improving lighting conditions;
- preparing meals;
- labeling medications, clothing, and appliances;
- writing;
- keeping financial records;
- personal grooming;
- using magnifiers for easier reading; and
- systematizing shopping and payment at the register.
Why Did I Need Low Vision Rehabilitation?
There are some very good reasons for low vision rehabilitation training, the most important being increased physical and psychological health. Research has shown that people with low vision tend to have more emotional difficulties and a higher risk of accidents than normally-sighted individuals. Patients who have undergone rehabilitation, however, have reported significant improvements in their functional abilities, a high rate of continued use of low vision devices, improvement in reading and distance vision, and general satisfaction with the quality of life.
When my right eye went bad, I couldn’t read, and I couldn’t drive. I couldn’t work in my wood shop, which bothered me a lot. I thought I was going totally blind. I became very depressed, and pretty much decided that life as I had known it was pretty much over.
There was more stress at home. The family couldn’t accept the fact that I couldn’t see well, and I just couldn’t help out, couldn’t do the carpentry, and couldn’t help my kids with building their houses. My wife, Marie, was very understanding, but it was difficult for her.
I tried to continue teaching. The students and staff were very supportive in the beginning, but they seemed to forget after a while. Writing lesson plans and grading papers was difficult. I particularly had problems with reading textbooks and journals.
Step #1: Evaluation
The first step in the rehabilitation process is working one-on-one with a counselor or specialist who will assess your needs and identify which programs are best suited to meet them.
My eye doctor referred me to the optometrist at the low vision clinic for evaluation. After my appointment was scheduled, a low vision therapist called me and asked me questions about my health, eye condition, and what she called my visual goals–the things I wanted to do, but couldn’t, because of my impairment.
Then, when Marie and I went to the clinic, the therapist talked with us about the problems I had that were caused by my poor vision. She explained how I could make the best use of my remaining sight through training, low vision devices, and services.
She said that together, she, the low vision team, and I would lay out a rehabilitation plan to help me meet my goals, and that my doctors would get reports as we went along. She told me that the program could take several visits over a few weeks, and that I would have to really want to succeed for it to work. Well, I did want to succeed–not just for myself, but for Marie and the kids–so I said, “Go for it.”
My initial visit was not what I expected. Rather than the kind of eye exam I had received from my medical eye doctor, the therapist put me through a battery of questions and tests to determine my functional needs, my visual capabilities and limitations, and any history of health problems and related treatment requirements that might affect my visual recovery.
Together, we developed a complete case history to determine how I was functioning and what my needs might be. This included an analysis of my reading habits and other near-vision activities, use of low vision devices, and incidents of eye strain or fatigue.
I had to answer many questions about such things as my ability to care for myself, the nature of my home environment, problems caused by my vision impairment, my employment situation, my relationships with family and friends, ways in which I have adapted to vision loss, and how well I’m doing mentally and emotionally.
I thought the questions would never end, but I knew how important they were. The rehab therapist didn’t leave any stones unturned, that’s for sure. I think, by the time she was through, she probably knew more about me than my own wife, and after 36 years of marriage, that’s saying a lot.
After analyzing the results of my initial evaluation, the vision team agreed that I was a good candidate for success through rehabilitation, and they began to devise a plan to fit my needs and goals.
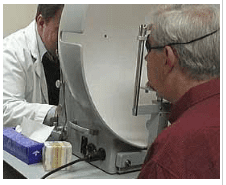
Step #2: Vision Assessment
The next step was for the low vision optometrist to assess my visual functions through tests and techniques which were adapted to fit my visual impairment.
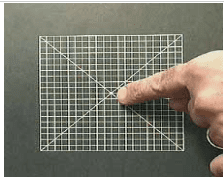
My visual acuity and refractive status were tested using special low vision refractive techniques. These tests made use of larger-than-usual testing charts, control of illumination, the use of trial frame refraction, and techniques that allow for eccentric, or off-center, viewing. The tester also used an Amsler grid, a simple way to identify defects in my central visual field;
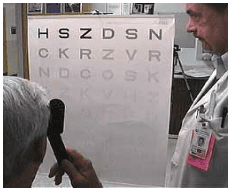
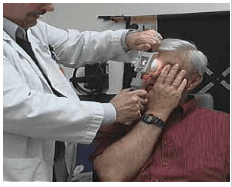
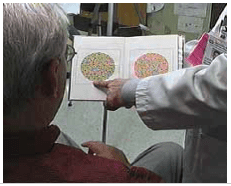
My visual field was analyzed in order to predict how I might function in day-to-day activities and how well I might respond to various rehabilitative approaches. Four types of visual field tests are available for this purpose:
A tangent screen test, during which the patient identifies a spot of light moving into his peripheral field.

A confrontations test, wherein the doctor introduces objects such as fingers or lights from the side to see if there are any large field defects like loss of side vision to one side due to stroke. This test is not sensitive to small or slight changes in the vision.

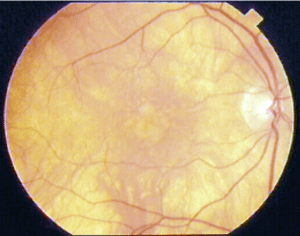
My test results confirmed that I had the exudative, or wet, form of macular degeneration with no other ocular complications. My condition had been first diagnosed as age-related macular degeneration at age 60. At that time, I had large and numerous deposits, called drusen, beneath the retina of both eyes, and my vision was distorted by the accumulation of this debris.

I agreed to attend weekly training at the center. My rehabilitation therapist and I established a list of personal visual goals that would give direction to my training. These goals were in the areas of activities of daily living (often called independent living skills), computer use, and counseling. Vocational rehabilitation might have been part of the program, but I was fortunate. Before my rehabilitation training began, I was able to retire early with full benefits. If I had needed to remain employed, several psychometric assessments would have been made to evaluate my current skills as they related to my teaching assignment or other areas of interest.
My training began with safe cooking strategies, labeling techniques, use of adaptive equipment, and an evaluation of the safety and lighting in my home.
Most of the training took place in a supervised program of self-care using a specially-designed apartment at the center.

I relearned everything. Things I had been doing my whole life I had to learn to do all over again, this time without depending so much on my eyesight. It wasn’t easy. I trained twice a week for six weeks, and each session lasted for one or two hours.
The first thing the therapist showed me was a system for recording phone numbers, and she enrolled me in the free phone service for visually-impaired people.
Then she showed me how to take care of my clothing and do the laundry in a whole different way. We labeled my clothing and all the appliances in several ways. Sometimes we just used large print, but she also showed me how to use some stuff that left a raised, high contrast line I could feel.
I learned how to sew and iron safely, including how to use a needle threader. And the therapist offered some good practical advice like wearing wrinkle-free clothes. I hate to iron, so that was a very good suggestion.
We got into personal grooming and hygiene, like brushing my teeth and taking care of my finger and toe nails. I never thought how tricky those things could be without good vision.
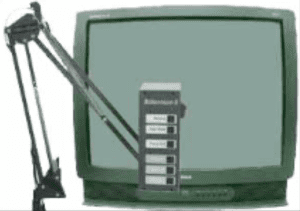
We worked on budgeting, including using a CCTV and a signature template for reading and paying bills. And now I carry a multi-compartment wallet for keeping my money denominations separate. That was a great idea.
My therapist had lots of good housekeeping tips, like assigning definite locations for cleaning equipment and tools, using disposable plates and utensils, and all kinds of things like that.
She taught me some practical eating skills, too, so I wouldn’t embarrass myself or Marie in a restaurant. I never thought I could use my fingers to eat with and still look classy.
I learned how to cook without burning the house down or losing a finger. I learned to take along a large-print grocery list and a hand magnifier when I go shopping. And one of the most important things she made sure I knew was where our basic medical supplies are and how to identify and use them.
The rehab therapist also worked with me in communications using large print, and in touch typing. I never could type without looking at the keys, but I’m pretty darned good now. They also got me two pairs of sun shields: one pair to cut down glare from artificial lighting, and another for bright sunlight.
I knew how to use a computer already, but I didn’t know about all of the magnification and speech software there is for the vision-impaired. During my residential training, the adaptive technology manager showed Marie and me the latest technology and let us try several different programs. I also know about several agencies and organizations where I can get adaptive software at no cost. Since I’m on retirement income now, that’s good to know.
My condition was not severe enough to require orientation and mobility training. A person with nearly total vision loss would require about 25 hours of individualized sessions by an O&M specialist, with advanced training in actual public situations. The activity would also include several hours of calisthenics and walking. Skills such as safe street crossings, negotiating stairs and curbs, and utilizing public transportation would be learned, in addition to familiarization with new environments. Use of an animal guide would also be an important consideration, as would training in Braille.
Both personal adjustment counseling and marital counseling were undertaken to help my family and me deal with my loss of vision. Counseling was a daily part of the team approach to my visual rehabilitation.
In general, I handled my vision loss well. The most difficult part was dealing with the changed dynamics within my family and with problems of communication with my children. Gradually, my self-esteem and confidence in my ability to overcome my vision impairment greatly improved.
During my training, weekly team meetings were held, with Marie in attendance. My progress was discussed, and program plans were reviewed. Direct lines of communication were constantly maintained between the rehabilitation center’s staff, the state sponsoring agency, my family, and me.
Low vision management was another important part of my rehabilitation. This centered around two areas: modification of my environment and possible treatment options with low vision devices.
Step #4: Environmental Modification
For patients with mild vision loss, simple environmental modifications may be enough to perform daily living tasks. Patients like me, with moderate to severe visual loss, will also benefit from environmental modifications, but we also need low vision devices to help maximize our vision.
Four factors were taken into consideration when analyzing my home: illumination, glare, contrast, and figure-ground perception.
Illumination
Lighting is probably the most important aspect of the environment for a vision-impaired person. It is also the easiest to modify.
Because of my vision impairment, I needed more light than normal. This was accomplished by increasing the number and power of the lamps and fixtures. For general lighting, floodlights and walkway lights were installed on the outside of the house. For near-vision tasks, gooseneck and swing-arm lamps with insulated reflector shades were placed at all work stations and reading chairs. Different types of bulbs (soft white, clear, etc.) were experimented with to decide which tints were more comfortable for me.
Glare
Next, the rehabilitation therapist helped me to identify potential sources of glare in my home. In just a few hours, they found and eliminated many areas of so-called “discomfort glare.” With Marie’s help and input, shades were added to windows on the sunny side of the house, scatter rugs were secured to the polished wood floor in the dining room, and I made cutout line guide for reading magazines with glossy pages.
I also keep my brimmed hat and my tinted and polarized glasses handy for any other situations that might occur, either indoors or out. These items are also helpful for occasions when veiling glare makes seeing difficult. Veiling glare is caused by scattering of light within the eye itself, which can result from high-intensity headlights and reflections from the sun in environments over which I have no control.
My retinal condition caused me to be photosensitive, even in lighting conditions that most people would consider to be normal. If my condition was such that my vision was even more seriously hampered by light, my specialist might have recommended soft contact lenses with central red or amber filters. As it stood, however, the changes made by my rehabilitation therapist went a long way toward improving my visual capabilities.
Contrast
Contrast makes it possible to differentiate an image from its background. It is very important to good vision. My rehabilitation therapist found many ways to enhance the contrast of my surroundings, which proved to be very helpful.
The changes they made in my home were simple, but effective. They included:
- Installing faceplates on electrical switches and outlets in contrasting color to the wall;
- Covering a glass-topped table with a dark-colored tablecloth;
- Applying dark-colored decals to a sliding glass door;
- Laying a dark-colored bath mat over the edge of the tub and placing a rubber ball in the bathtub to help me see the water level;
- Wrapping rings of bright tape around handles of pots, tools, and utensils; and
- Applying white paint to the leading edge of the porch steps.
Figure-ground perception
Finally, the rehabilitation therapist had a look at my wood shop. She found my project table to be a victim of “figure ground” or “visual clutter.”
Simply put, it required organization so that I could find what I needed without being visually confused by a number of other objects. The therapist also recommended painting the table top a solid, non-glossy light color to make it even easier to locate parts and pieces.
The therapist complimented me on already having my tools fairly-well organized on peg boards, and smaller items, such as nails and screws separated into drawers for easy identification.
Step #5: Low Vision Devices
Magnification of both near and distant images can improve visual function in nearly all patients with central vision loss. I was was amazed at the variety of low vision devices that could help me to maximize my sight.
Back at the center, I was given hands-on experience on almost every kind of device imaginable. This included typical optical aids, such as prescription magnification or microscopic glasses;
. . . filters to reduce glare and increase contrast;



I was especially impressed with a scanner that could be combined with computer software to read printed text aloud. Nowadays, those are combined into single units called “optical character recognition” (OCR) devices.
I was computer-literate, having used one for years in my teaching. But I had no idea this kind of technology was so easily available to me.
As a result of rehabilitation, I eventually found the low vision devices most suitable to my needs. Then came careful training in the correct usage of the devices. The adaptive technologist gave me large-print instruction sheets to take home, and I was grateful that she didn’t expect me to remember every detail.
The purpose of low vision devices is to maximize sight. This is done through magnification for people who have central vision loss like I do, and field expansion for people who have peripheral vision loss.
A doctor who specializes in low vision knows about the different types of magnification and the circumstances in which each is used. In other words, when to use angular magnification (such as a telescope or bioptic eye wear), rather than relative distance magnification (such as a hand-held magnifier). Or when to use relative size magnification (such as large print), rather than projection magnification (such as a closed circuit television) .
The specialists at the center keep up on the latest technology, so I knew that I was receiving the best information and training available for my unique needs.
In order to select the most appropriate low vision devices, the specialists had to:
- Identify exactly what tasks I wanted to accomplish.
- Analyze my fine and gross motor skills to confirm my ability to operate the low vision devices.
- Determine which of my eyes was dominant.
- Determine whether I would do best with monocular or binocular vision.
- Determine whether I could learn to enhance my vision in a new healthier area of my retina, called the “preferred retinal loci,” or PRL.
- And finally, determine whether my need for higher-than-normal lighting levels would require illuminated magnifiers.
They figured out exactly what I need to see better and to live an almost normal life again. For closeup viewing, they gave me an illuminated hand-held magnifier and a stand magnifier.
For reading, which I though I’d never get to do again, I got a basic table-top CCTV. It has a magnification range that fits my acuity. That was good thinking.
For my computer I got large-print, white-on-black labels for the keys. I got a scanner with screen reader software, a new 19-inch monitor, software that magnifies the screen and the cursor, and now that machine can even recognize my voice and type for me.
As if that wasn’t enough, my optometrist fitted me with prescription lenses just for using the computer, and they’re tinted specially to take care of eye strain. Then they gave me a little telescope for reading street signs, identifying people, and seeing the sights. It took some practice getting used to it, but it’s worth it.
There are all kinds of what they call non-optical devices, too. Marie and the kids went shopping for my birthday out of one of those catalogs, and I actually use everything I got. Even stuff I didn’t know I needed, like a talking watch. And a gadget that actually tells me when my cup is getting full so I don’t pour coffee all over the table any more. I can’t wait until Christmas now.
Finding a Low Vision Rehabilitation Center
I was fortunate to have an outstanding rehabilitation center near my home. The center offered comprehensive programs with teams of occupational therapists trained in visual rehabilitation, vocational rehabilitation counselors, vision rehabilitation therapists, orientation and mobility specialists, psychologists, assistive technology computer specialists and other professionals as needs dictate.
Such teams can be found in some university centers and large private clinics. Rehabilitation services may also be provided by charitable organizations such as Lighthouse International, the Jewish Guild for the Blind in New York City, Alphapointe Association for the Blind in Kansas City, and the St. Louis Society for the Blind. The VICTORS program under the Veterans
Administration is an excellent regional rehabilitation service for veterans.
All state governments in the United States fund an agency to coordinate the visual rehabilitation of its vision-impaired citizens. They take care of most of the rehabilitative efforts, either directly or through subcontractors. Called either “Rehabilitation Services for the Blind” or “Commissions for the Blind,” these organizations can be found listed by state in the “Resources” section of the MD Support web site at www.mdsupport.org.
In cases where a person might not meet the eligibility requirements of the state blindness agency, but the person’s employment is being adversely affected, they can go for help to the state’s vocational rehabilitation agency, also listed in the MD Support resources.
Paying for Low Vision Rehabilitation
How did I get the help I needed, and how was it paid for? The referral mechanism differs slightly with each state, but generally, a referral can be requested by any individual, family, friend, eye care professional, rehabilitation specialist, or social worker.
State statutes specify the minimum levels of vision loss for entry into the program, but there is also some flexibility in the acceptance standards. A doctor must provide documentation of the best-corrected visual acuity and/or the visual field in each of the patient’s eyes.
State agencies will usually cover the costs of rehabilitation for people who are registered. Those who are not qualified for government assistance might expect to pay their own expenses.
Government agencies do the best they can with the limited funds available, and private or non-profit organizations help to fill the gap. The task, however, is much larger than current budgets and resources allow.
According to the Alliance for Aging Research, vision impairment is one of the four leading causes of lost independence among older people, with annual costs for medical and long term care in the billions of dollars. Low vision rehabilitation can cut these costs considerably by helping to restore functional abilities, safety, and independence.
Conclusion
Since my initial low vision assessment and training, I have greatly improved my skills for independent functioning. My social life has slowed somewhat, not so much because of my vision impairment, but because of my retirement from the school system. Marie and I still go out when our budget allows, and we enjoy the closeness and support of our active family.
Vision rehabilitation isn’t easy, and it isn’t a cure for blindness. It’s an educational process that requires patience, practice, flexibility, and motivation. And it requires a team of professionals who know what they’re doing and who care about you as an individual.
The specialists and doctors at my rehab center were good, but they could be only as good as I would let them be. As I always told my students, if a person doesn’t have a real reason to want to learn–a ton of self-motivation–then there isn’t anyone who is going to be able to teach them.
It was a long road, but I don’t even want to think how long the rest of this road would be without the confidence and independence those people have given me. They gave me the tools, taught me how to use them, and showed me that my life can be just as good as it always was. Different, maybe–not like I thought it was going to be–but it’s good.
Copyright 2002, Dan Roberts
Credits
Script & Video: Dan Roberts
Script Consultants:
Roy Gordon Cole, O.D., F.A.A.O. (Director of Vision Program Development, The Jewish Guild for the Blind, New York, NY)
Brian Gerritsen, M.A., CLVT (Rehabilitation Specialist, Low Vision Rehabilitation Services, North Ogden, UT)
Joseph Maino, O.D., F.A.A.O. (Chief, VICTORS Low Vision Rehabilitation Program, Kansas City VA Medical Center)
Clay Berry (Assistant Director of Rehabilitation, Alphapointe Center for Blindness and Low Vision, Kansas City, MO)
Information sources:
- Alliance for Aging Research
- American Optometric Association
- Bossert Specialties, Phoenix, AZ (photos: low vision devices)
- Center For The Partially Sighted, Santa Monica, CA
- Susan E. Edmonds, O.D. (author: What is Low Vision Rehabilitation, published at www.edmondsgroup.com/practices/vision.htm)
- Hippocrates Home magazine
- Lighthouse International
- Missouri Rehabilitation Center for the Blind
- The New England Eye Center
- L. David Ormerod, MD, Sue Mussatt, RN, and Associates (authors: Low Vision Assessment and Rehabilitation, School of Health Professions and School of Medicine, University of Missouri, Columbia)
- University of Iowa Center for Macular Degeneration
- Richard L. Windsor, O.D., F.A.A.O. and Laura K. Windsor, O.D. (authors, Low Vision Rehabilitation: An Introduction, published in the Rehabilitation Professional Journal, Spring 2001.)